Excessive Daytime Sleepiness In Pd
Excessive daytime sleepiness is a common symptom in PD and can occur anywhere from 15 to 21% early in the disease course and up to 46% as the disease progresses . A study of early and untreated PD showed that EDS may be related to disease progression and is independent of other sleep disorders, while others have shown that dopaminergic medication appears to increase EDS in a dose-dependent fashion . Some studies have also suggested an association of EDS in PD with depression . Interestingly, patients with PD and EDS appeared to have reduced uptake in the basal ganglia on dopaminergic terminal imaging compared to those without EDS . The PD and EDS groups also have worse scores on motor, nonmotor, autonomic, and cognitive testing . This suggests that more severe disease could be a contributing factor to development of EDS, in addition to dopamine medication levels .
The presence of EDS negatively impacts quality of life in PD. One study evaluated 198 patients with PD using the Parkinsons Disease Questionnaire 39 , a measure of quality of life . This study demonstrated that those with PD and EDS had a significantly lower overall score on the PDQ-39 than those without EDS , as well as individual emotional, social, and physical domains measured by this survey . EDS in PD also represents an additional risk of falling. One study evaluated 120 patients with PD and found that every point increase on the Epworth Sleepiness Scale was associated with a 20% higher risk of falling .
Before Going To Bed Avoid Caffeine
Tea, coffee, chocolate, and cocoa are included in this category. It is important to check the label of soft drinks to determine whether they contain caffeine. You can feel more awake when you consume caffeine, which is a stimulant.
Its effects may last for three to four hours. At bedtime, caffeine can affect your body by increasing the time it takes you to fall asleep and making you sleep lighter and more restless. As well as limiting your intake of caffeine during the day, it is also important to limit your total intake.
Buy Modalert 200 Tablet may help you sleep better.
Sleep Benefit And Positive Effect Of Sleep Deprivation In Patients With Pd
The complex interaction of sleep and motor function is reflected in two interesting phenomena: sleep benefit, i.e. the experience of an improvement of motor function upon awakening , and a positive effect of sleep deprivation on motor function .
Sleep benefit was first described based on patients reports, and systematically evaluated in large cohorts of patients with PD with contrasting results. Some groups reported this phenomenon to be common in a subgroup of PD patients with specific clinical characteristics, e.g. with longer disease duration and younger age at onset of disease . This phenomenon has been reported to be so relevant to allow PD patients with sleep benefit to skip or delay medication . A study systematic evaluating motor state a night before sleep and in the morning upon awakening reported a slight motor improvement in the morning in patients with sleep benefit, without polysomnographic differences between the two groups . Another study using PSG reported shorter total sleep times and longer sleep latencies in PD patients reporting sleep benefit .
However, other groups found no actual improvement in motor functioning in PD patients reporting sleep benefit , or only in a small percentage of them , or reported in those patients with PD experiencing sleep benefit no association with the previously reported clinical variables , maybe because of methodological issues.
You May Like: Parkinson Disease And Tooth Extraction
Read Also: How Do You Diagnose Parkinson’s Disease
Evaluation Of Sleep Hygiene Program: Sleep Diary
Monitoring the effectiveness of behavior changes is best done by keeping a diary. The table below depicts a sample diary that could be kept by the bedside and filled out upon arising by the patient or caregiver. If daytime sleepiness and napping are problems, items can be added to record the number, time, and duration of napping episode. The diary can be carried with the patient.
Recommended Reading: Loss Of Balance Parkinson Disease
The Need For An Instrument Such As The Pdss
Work from our own group and others indicates that the aetiology of nocturnal disabilities in Parkinsons disease is multifactorial and that nocturnal motor symptoms are of importance. Traditionally, sleep assessments in Parkinsons disease have taken the form of pure subjective questioning or, in some cases, measurement of sleep architecture. These techniques, however, do not provide a holistic assessment of the night time problems of sufferers from Parkinsons disease. It can be arguedgiven the importance of sleep function in this diseasethat assessment of night time problems requires a specific instrument similar to the UPDRS. The PDSS aims to provide this. Some currently available tools, including the ESS, only address single items such as excessive daytime sleepiness and are thus not comprehensive. In a study of excessive daytime sleepiness and its potential relation to sudden onset sleep in 638 patients with Parkinsons disease, Lang et al recently concluded that the ESS has poor sensitivity for predicting falling asleep while driving, and may not be appropriate for assessing susceptibility to unintended sleep episodes. Other studies have indicated that ESS scores do not correlate significantly with multiple sleep latency test scores, thought to be the gold standard for measuring sleep, and especially REM sleep latency during the daytime. Thus we feel the PDSS may offer a more practical and relevant way of assessing sleep disruption in Parkinsons disease.
Don’t Miss: Does Parkinson’s Affect The Mind
Rem Sleep Behavior Disorder
REM stands for rapid eye movement. This is the stage of sleep when dreams take place. People with REM sleep behavior disorder act out their dreams, which can be violent. RBD is one of the early warning signs of Parkinsons. Healthy people with RBD have a higher risk of developing Parkinsons. RBD can be treated with the drug clonazepam .
Hallucinations And Rem Sleep Disorders In Parkinson’s Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
Also Check: Anticholinergics For Parkinson’s Disease
Sleep And Parkinsons Disease
The Palo Alto Parkinsons Disease support group February 2020 meeting featured Dr. Emmanuel During, a Stanford sleep medicine neurologist. During the meeting, Dr. During discusses sleep disturbances that can occur in PD, such as insomnia, restles legs syndrome, sleep apnea, and REM sleep behavior disorder , along with available treatments. There’s a question and answer session.
How Is Psp Diagnosed And Treated
Diagnosing PSP
Currently there are no tests or brain imaging techniques to definitively diagnose PSP. A physician will review your medical history and perform a physical and neurological exam. Identifying early gait problems, problems moving the eyes, speech and swallowing abnormalities, as well as ruling out other similar disorders is important. Diagnostic imaging may show shrinkage at the top of the brain stem and help doctors examine brain activity in known areas of degeneration.
Treating PSP
Currently there are no effective treatments for PSP and symptoms usually do not respond to medications.
- Parkinson’s disease medications, such as ropinirole, rarely provide additional benefit. In some individuals, other antiparkinsonian medications, such as levodopa, can treat the slowness, stiffness, and balance problems associated with PSP, but the effect is usually minimal and short-lasting.
- Botulinum toxin, which can be injected into muscles around the eyes, can treat excessive eye closing.
- Some antidepressant drugs may offer some benefits beyond treating depression, such as pain relief and decreasing drooling.
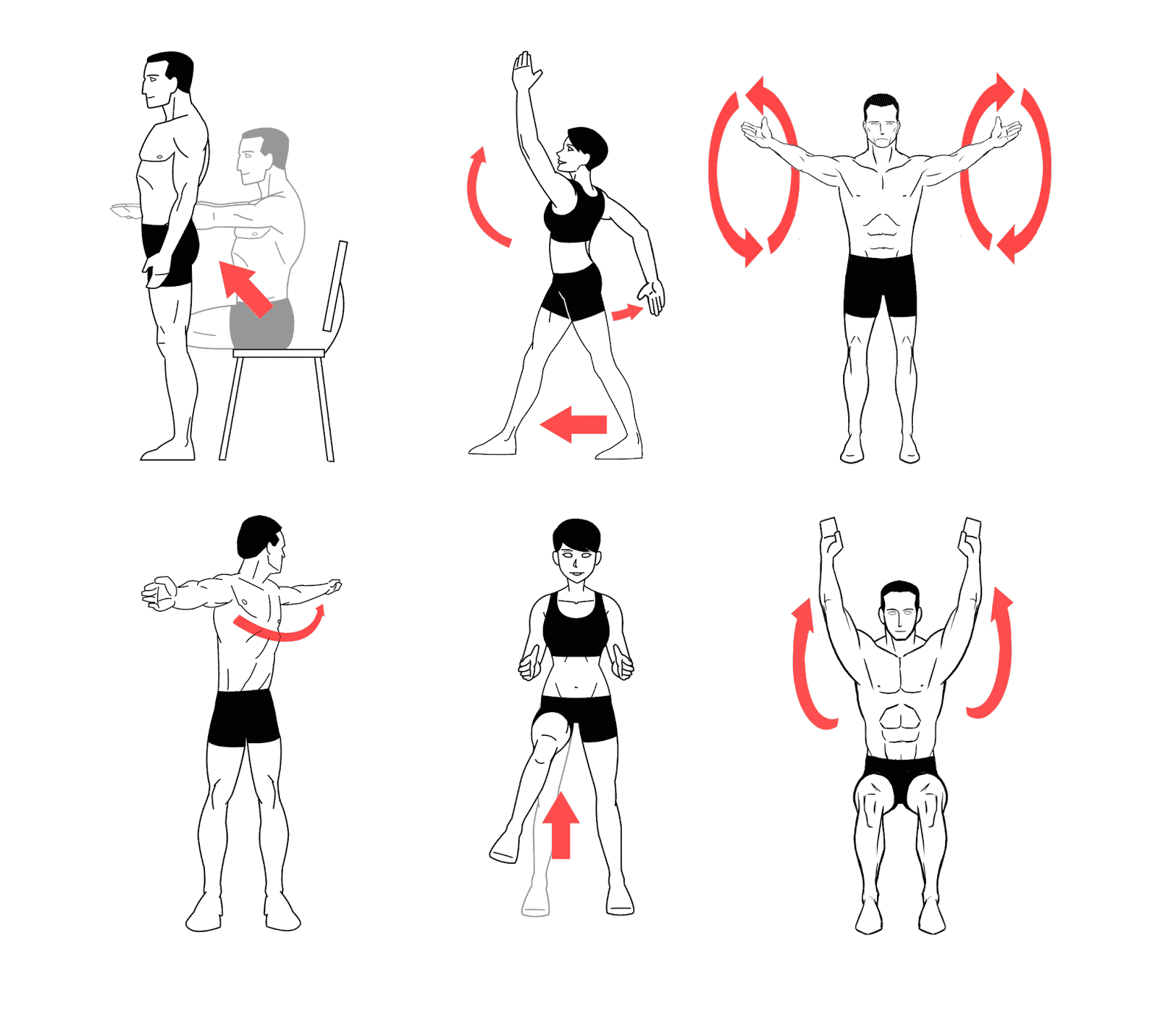
Non-drug treatment for PSP can take many forms.
- Weighted walking aids can help individuals avoid falling backward.
- Bifocals or special glasses called prisms are sometimes prescribed to remedy the difficulty of looking down.
- Exercise supervised by a healthcare professional can keep joints limber but formal physical therapy has no proven benefit in PSP.
Read Also: How To Talk To Someone With Parkinson’s
Good Night: Sleep And Parkinsons Disease
Lack of good sleep can worsen Parkinsons symptoms. In this 45-minute lecture, Dr. Rafael Zuzuárregui addresses causes of sleep loss and the latest treatments for: insomnia, restless leg syndrome, REM sleep behavior disorder, nocturnal urination, hallucinations, wearing off of medication, dystonia and sleep apnea.
Recommended Reading: How Long Does Parkinsons Last
Nighttime Hallucinations Psychosis & Confusion
Nighttime hallucinations and confusion may result from any combination of cognitive impairment, dopaminergic medications, age and PD-related vision changes and lack of sleep. Psychosis may first appear after infection, trauma, surgery or prolonged hospitalization. Symptoms may range from a sensation that someone or something is standing at the side of or behind the person, to very detailed and often frightening visions. Delusions may occur as well.
Treating Parkinsons Psychosis
The first-line approach to treatment of PD psychosis involves simplification of the anti-PD medication regimen and adjusting dose timing , treating other sleep disturbances, providing a consistent and familiar sleep environment , and in more severe cases, the use of atypical antipsychotic drugs.
Most of the available anti-psychotics are always avoided in PD psychosis because they block dopamine receptors and can cause significant problems with movement. However, two anti-psychotic medications, quetiapine and clozapine, are sometimes used as they have less of an ability to worsen motor symptoms. However, data for the use of quetiapine is limited and clozapine requires the patient to undergo frequent blood draws to monitor blood counts. A newer medication pimavanserin, was approved by the FDA to treat PD psychosis. It has a different mechanism of action, and does not block the dopamine system, but rather the serotonin system, and therefore does not increase motor symptoms.
Also Check: Lewy Body And Parkinson’s
When Should I Call My Healthcare Provider
Reach out to your provider if trouble sleeping harms your quality of life. Always call your healthcare provider if you experience symptoms that worry you, especially if they could put you or those around you in danger.
Sometimes, a sleep disturbance could be a sign of depression related to Parkinsons disease. If youve lost interest in activities you once loved or feel numb to whats going on in your life, reach out to a provider you trust. Some people feel better after starting a new medication or talking to someone about what theyre feeling. You dont have to feel like this.
A note from Cleveland Clinic
Researchers continue to study the sleep-Parkinsons disease relationship. Understanding more about how Parkinsons affects sleep may lead to earlier detection of Parkinsons disease and more effective treatments. Even now, you have plenty of options to treat sleep problems. Be open with your provider about any sleep issues youre having. Together, you can find a plan that improves your sleep as well as any other challenges Parkinsons disease may create in your life.
Also Check: Can An Mri Detect Parkinsons
What Are The Latest Updates On Psp
The National Institute of Neurological Disorders and Stroke , a component of the National Institutes of Health, is the primary funder of research on the brain and nervous system. NIH is the leading funder of biomedical research in the world.
PSP is one of the diseases being studied as part of the NINDS Parkinson’s Disease Biomarkers Program. This major NINDS initiative is aimed at discovering ways to identify individuals at risk for developing Parkinson’s disease and related disorders, and to track the progression of these diseases. NINDS also supports clinical research studies to develop brain imaging that may allow for earlier and more accurate diagnosis of PSP.
Understanding genetics and the tau protein
Genetic studies of PSP may identify underlying genetic causes. Previous studies have linked regions of chromosomes containing multiple genes, including the gene for the tau protein , with PSP. Researchers hope to identify specific disease-causing mutation and are also studying how genetics and the environment interact to make people more susceptible to the disease.
Developing treatments
Because the symptoms of PSP progress more rapidly than in other tau-related disorders, some investigators believe that an anti-tau therapy will show benefit rather quickly in PSP clinical trials. Many of these anti-tau therapies make use of treatments that help the immune system fight infections and other diseases.
Treating symptoms of PSP
Read Also: How To Be Diagnosed With Parkinson’s Disease
They Can Be An Indicator Of Mental Health Problems
anxiety, stress or depression They can bring with them recurring nightmares.
They are also a core symptom of PTSD, perhaps because the difficulty withthat traumatic events are rooted in peoples inability to processs, refers to BBC Neil Greenberg, Advocacy Professor of Mental Health at Kings College London. So what happens is that your mind unconsciously tries to play with them, tries to understand them.
Data from the University of Pittsburgh School of Medicine, published in 2009 Sleep Medicine ClinicIt has been shown that up to 80% of people with PTSD have frequent nightmares.
Research suggests that adversity, especially in childhood, can affect the ability to regulate emotions and contribute to these spontaneous and intense anxiety dreams.
Studies have also shown other mental health problems are often associated with nightmares, such as: bipolar disorder and schizophrenia,
Clinical Features Of Insomnia
Insomnia is defined as difficulties initiating sleep , sleep maintenance problem or early awakening . In studies, it has been reported that the frequency of insomnia in patients with PD varies from 27 to 80% . It has been reported that the most common types of insomnia in PD patients are sleep fragmentation , and early awakenings . It has been reported that insomnia may occur alone or accompany comorbid mental or systemic illnesses, and it is associated with disease duration and female gender . Sleep fragmentation is defined as a deterioration of sleep integrity , and it leads to a lighter sleep or wakefulness . In studies, it has been reported that sleep fragmentation is the most common sleep disorder in patients with PD .
Read Also: How To Avoid Getting Parkinson’s
Sleeping With The Enemy
Sleep disorders are one of the most common problems experienced by people with Parkinsons Disease. A major study concluded that more than 60% of people with PD experience sleep-related difficulties, with this percentage rising based on the length of time living with the disease.
Insufficient sleep can severely impact quality of life, and exacerbate other PD symptoms.
Like many other aspects of PD, while many people have sleep problems, they do not all have the same type of sleep disturbances.
If you want to improve your sleep, it is important to understand the type of sleep disturbance that you experience. This will allow you to focus on tips and solutions that are most relevant for you, and to better communicate your problems with your doctor.
Ive found this presentation by Dr. Jason Valerio and published by the Parkinsons Society of British Columbia to be extremely helpful.
Its a rather long video, but its worth watching, and then rewatching.
The first time you watch the video, concentrate on learning a broad overview of the different sleep disorders that are commonly associated with PD. That will help you understand what sleep problems you experience. It is then worthwhile to rewatch the video to concentrate on the tips and suggestions that are applicable to your sleep problems.
Broadly speaking, sleep issues are categorized into one or more of the following categories:
- Difficulty Falling Asleep
- Difficult Staying Asleep
- Excessive Daytime Sleepiness
Parkinson Canada
Hallucinations And Rem Sleep Disorders In Parkinsons Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
Recommended Reading: What Is The Etiology Of Parkinson’s Disease
What Causes Parkinsons Disease
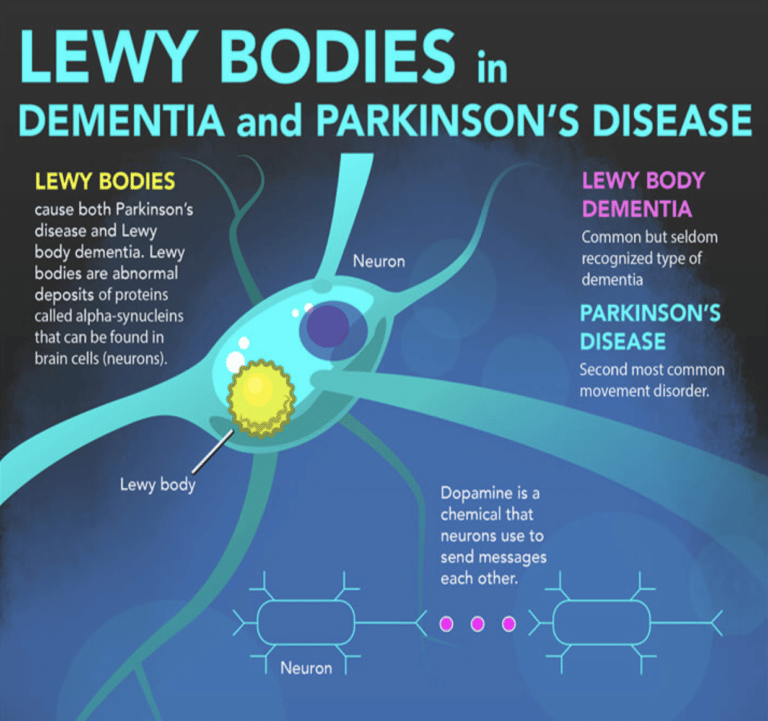
The most prominent signs and symptoms of Parkinsons disease occur when nerve cells in the basal ganglia, an area of the brain that controls movement, become impaired and/or die. Normally, these nerve cells, or neurons, produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems associated with the disease. Scientists still do not know what causes the neurons to die.
People with Parkinsons disease also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinsons, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying position.
Many brain cells of people with Parkinsons disease contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinsons andLewy body dementia.
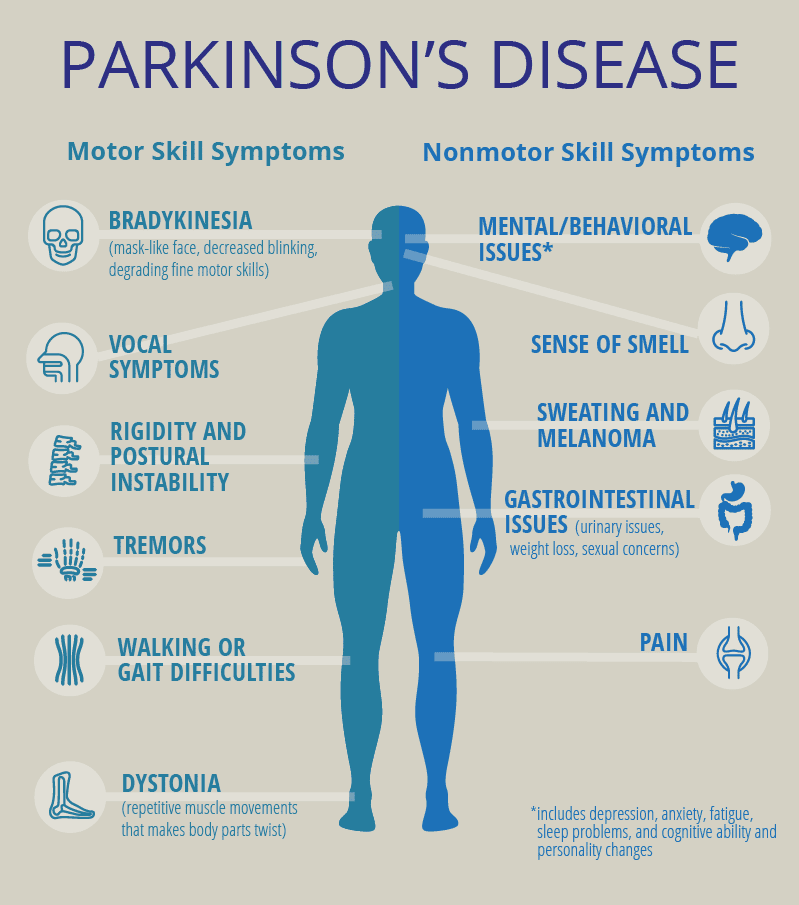
Parkinsons Disease: Causes Symptoms And Treatments
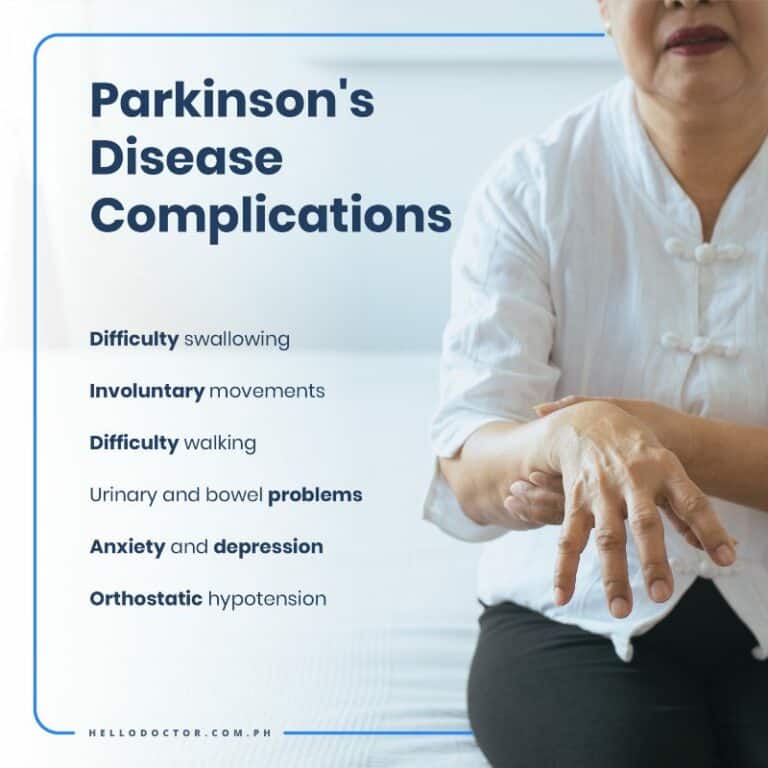
Parkinsons disease is a brain disorder that causes unintended or uncontrollable movements, such as shaking, stiffness, and difficulty with balance and coordination.
Symptoms usually begin gradually and worsen over time. As the disease progresses, people may have difficulty walking and talking. They may also have mental and behavioral changes, sleep problems, depression, memory difficulties, and fatigue.
While virtually anyone could be at risk for developing Parkinsons, some research studies suggest this disease affects more men than women. Its unclear why, but studies are underway to understand factors that may increase a persons risk. One clear risk is age: Although most people with Parkinsons first develop the disease after age 60, about 5% to 10% experience onset before the age of 50. Early-onset forms of Parkinsons are often, but not always, inherited, and some forms have been linked to specific gene mutations.
Read Also: Men’s Shoes For Parkinson’s Patients
source https://www.parkinsonsinfoclub.com/parkinsons-and-sleep-problems/