Sensitivity Specificity And Predictive Value Of A Previous Diagnosis Of Parkinson’s Disease
Of 126 patients with a pre-existing clinical diagnosis of probable and possible Parkinson’s disease in the overall sample , 111 were confirmed as having Parkinson’s disease, resulting in a sensitivity of 88.1% similarly, it was confirmed that 54 of 74 patients did not have Parkinson’s disease, resulting in a specificity of 73.0% . The positive and negative predictive values of a previous clinical diagnosis of Parkinson’s disease were 84.7% and 78.3% . In other words, in 85% of patients with a previous diagnosis of Parkinson’s disease this diagnosis was confirmed, and 78% of patients with a diagnosis other than Parkinson’s disease did not have the disease .
When this was broken down by a specialist or other doctor diagnosis, the diagnostic validity was as follows. Neurologists and geriatricians had a sensitivity and specificity of 93.5% and 64.5% , respectively, compared with 73.5% and 79.1% for non-specialists. The positive predictive values were greater for specialists than for other doctors , but the negative predictive values were equivalent v non-specialist 79.1% ).
Evaluation Of Publication Bias
Deeks funnel plots were produced to explore the potential presence of publication bias. Based on the symmetric shape of the funnel plot of pooled DOR and the Deeks test non-significant value , there is no potential publication bias in the current meta-analysis.
Funnel plot for the assessment of the potential publication bias of the 31 included studies.
Each solid circle represents each study in the meta-analysis. The line indicates the regression line.
Pharmacological Treatment Of Parkinson’s Disease
There is currently no proven disease-modifying or neuroprotective therapy for PD. A summary of previous neuroprotection trials is given in a recent review article. Current evidence-based treatment for PD is symptomatic and mainly based around dopaminergic replacement or modulation . The evidence base is summarised in recent guidelines from the National Institute for Health and Care Excellence and the International Parkinson and Movement Disorder Society. Levodopa, dopamine agonists and monoamine oxidase B inhibitors are all licensed for use as initial therapy in PD. Anticholinergics are no longer routinely used due to the risk of cognitive decompensation.
Pharmacological therapies currently used for initial and adjunctive treatment of motor symptoms in Parkinson’s disease
You May Like: Can You Test For Parkinson’s Gene
Diagnosis Of Parkinson Disease: Motor Symptoms
The clinical diagnosis of Parkinson’s disease is based on the presence of characteristic motor symptoms: bradykinesia, rigidity, postural instability, and resting tremor but neuropathology is still considered the gold standard for definite diagnosis. Differentiating PD from other movement disorders can be challenging throughout the disease course, because signs and symptoms often overlap. Indeed, neuropathology studies reveal that clinical diagnosis of PD can be confirmed with an accuracy of about 75%. Good response to levodopa is often used to support the diagnosis of PD. However, cases of pathologically proven PD with poor response to levodopa have also been reported.
Misdiagnosis of PD can occur for several reasons. In a community-based study of patients taking antiparkinsonian medication, the most common misdiagnosis were essential tremor, Alzheimer’s disease, and vascular parkinsonism. In addition, many of the prominent features of PD may also occur as a result of normal aging or from comorbid and multifactorial medical conditions .
R. Savica, … G. Logroscino, in, 2016
Idiopathic Basal Ganglia Calcification
This is a heterogenous disease associated with mineral deposition in the basal ganglia, as well as in other brain structures. There is a strong familial component, with causative mutations identified in SCL20A2 and PDGFRB. Patients commonly have a movement disorder, with parkinsonian features of akinesia and rigidity which show a variable response to levodopa. Other features include cognitive impairment, gait disorder, pyramidal signs, and a psychiatric presentation. Imaging is crucial in diagnosis to identify the areas of calcification, with CT imaging being more useful than MRI .
Don’t Miss: Tests To Confirm Parkinson’s Disease
Tests To Rule Out Other Conditions
Blood tests can help rule out other possible causes of the symptoms, such as abnormal thyroid hormone levels or liver damage.
An MRI or CT scan can check for signs of a stroke or brain tumor, which may cause similar symptoms.
Hydrocephalus due to atrophy can occur with some types of dementia and would be visible with one of these imaging tests. If the person has neurologic symptoms but a normal scan result, Parkinsons disease may be present.
The doctor a lumbar puncture to rule out inflammation or a brain infection.
Patients With A Previous Diagnosis Other Than Parkinson’s Disease
Among all patients seen, two were referred for diagnostic purposes without a previous diagnosis, and 69 of 202 patients had a previous diagnosis other than Parkinson’s disease . Among these, 56 patients had been given a diagnosis of non-parkinsonian tremor, two of vascular parkinsonism, one of atypical parkinsonism, and 10 had been prescribed an antiparkinsonian drug for parkinsonian features without a specific diagnosis . Thirteen of the 69 patients with different diagnoses and the two patients referred for diagnostic purposes fulfilled strict clinical criteria for Parkinson’s disease . In two additional patients who had a previous diagnosis of non-parkinsonian tremor, a diagnosis of possible Parkinson’s disease was made . If only patients who had at some point in the past seen a specialist were considered, the diagnosis was changed to probable Parkinson’s disease in five and to possible Parkinson’s disease in one .
Sensitivity, specificity, and predictive values for the overall sample* and by type of clinician
You May Like: Does Mark Levin Have Parkinson’s Disease
What Is A Datscan And What Role Does It Play In A Parkinsons Diagnosis
In 2011, the FDA approved the use of a scan called a dopamine transporter scan . A DaTscan is an imaging technology that allows visualization of the dopamine system in the brain. It is similar to an MRI, but looks at the function of the brain rather than the structure.
A DaTscan involves injection of a small amount of a radioactive drug that is then measured by a single-photon emission computed tomography scanner . The SPECT scanner measures the levels and location of the drug in the brain.
It is important to know that a negative DaTscan does not rule out PD, especially early in the disease, but a positive DaTscan can help confirm it. A positive DaTscan can differentiate PD from essential tremor as there is no dopamine deficiency in the latter. However, DaTscan abnormalities can be seen in PD as well as other forms of atypical parkinsonism that cause a loss of dopamine . This means that a positive result does not differentiate Parkinsons disease from other forms of atypical parkinsonism.
Pd Diagnosis Disease Severity And Disease Progression
The diagnosis of PD is essentially clinical , and we believe that the clinical evaluation of patients will not be replaced by modern imaging techniques. Nevertheless, as pointed out earlier, misdiagnosis can approach 20% of cases . Recently, in line with the European Union, the U.S. FDA approved DAT scan as a diagnostic tool to help differentiate between PD and Essential Tremor. This is the only current FDA-approved subsidiary examination to aid in PD diagnosis.
The role of magnetic resonance imaging in the diagnosis of PD is still not fully established. Traditionally, it has been seen as a means to potentially exclude alternate diagnoses such as vascular parkinsonism, or more importantly , atypical forms of degenerative parkinsonism such as MSA or progressive supranuclear palsy . Traditional structural MRI findings of these latter diagnoses such as increased pallidal iron, rim of putaminal hyperintensity, hot cross bun sign and/or cerebellar atrophy in MSA or the hummingbird or penguin sign in PSP may not be reliable, particularly in early disease.
Figure 5. Multimodal MRI in PD. Differences are noted between patients with PD and controls through voxel-based analysis of R2, mean diffusivity, and fractional anisotropy maps.
-
Low dopamine transporter uptake in basal ganglia demonstrated by SPECT or PET imaging.*
Brent A. Vogt, in, 2019
You May Like: What To Say To Someone With Parkinson’s Disease
Progression Of Parkinson’s Disease
The disease progression of PD from diagnosis has been conceptualised into four stages . It is also important to recognise a prodromal phase in which non-motor symptoms, such as anosmia, constipation and rapid-eye-movement sleep behaviour disorder may predict the development of motor PD. Motor complications are more common as PD progresses, and typify transition to the complex phase. Many so-called axial symptoms of later stage PD, such as dysphagia, gait disturbance and falls, do not respond to levodopa, but may be helped by multidisciplinary team input. Dementia occurs in up to 80% of people with PD after 20 years disease duration. The rate of PD progression is heterogeneous and is generally more rapid in those with older age and more severe motor impairment at onset.
Stages of Parkinson’s disease. RBD = rapid eye movement sleep behaviour disorder.
The Diagnosis Of Idiopathic Parkinsons Disease
The first component to the diagnosis of PD is establishing that the patient has parkinsonism. This is a clinical diagnosis and relies on three key elements: bradykinesia, tremor, and rigidity. Of these, bradykinesia must be present, with at least one of the other two. PD is an asymmetrical condition, so during the clinical assessment, the parkinsonism should be more apparent on one side and may be purely unilateral in early disease . is a classical illustration of parkinsonism, with a description by William Gowers.
A case of Parkinsons disease as described and illustrated by William Gowers: the aspect of the patient is very characteristic. The head is bent forward, and the expression of the face is anxious and fixed, unchanged by any
Don’t Miss: What Is The Difference Between Parkinson’s Disease And Essential Tremors
Validation Of The Movement Disorders Societys Clinical Criteria Of Parkinsons Disease
Study Rationale:Diagnosis of Parkinsons disease and other causes of parkinsonism is not always an easy task for physicians. An accurate diagnosis, however, is an essential aspect of care for people with Parkinsons and of research trials, where the inclusion of incorrectly diagnosed patients can result in trial failure. Recently, the International Parkinson and Movement Disorders Society created new standard diagnostic criteria to improve the reliability of diagnosis. In this study we will test the validity of these criteria for diagnosing PD.
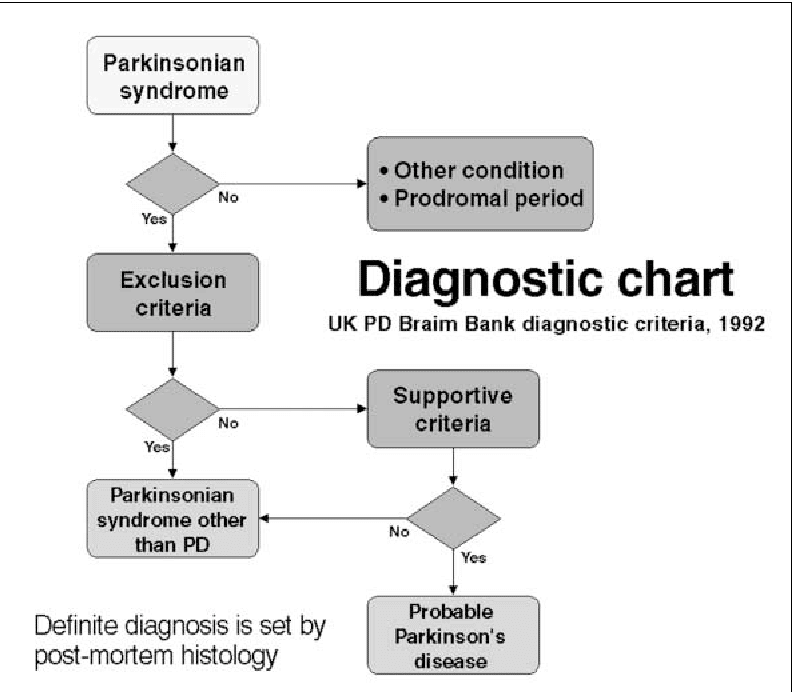
Hypothesis:We will assess the diagnostic value of the new MDS criteria and test them against the diagnosis of an expert and the previously established UK Brain Bank Criteria.
Study Design:The MDS criteria will be tested on 600 patients from 10 centers on different continents. After a phase of cognitive pretesting, during which the criteria are applied to a small group of people with PD, patients with a diagnosis of parkinsonism will be evaluated both by a clinical expert and a resident applying the new criteria as well as the UK Brain Bank Criteria. In a follow-up visit two years later, the diagnoses will be reevaluated.
Impact on Diagnosis/Treatment of Parkinsons Disease: These new criteria have the potential to facilitate and standardize the diagnosis of Parkinsons disease to detect patients with PD earlier and more reliably for earlier treatment and accurate involvement in trials.
Diagnosis Of Parkinson’s Disease
![[PDF] 1 Diagnosis and Differential Diagnosis of Parkinson â s Disease ...](https://www.parkinsonsinfoclub.com/wp-content/uploads/pdf-1-diagnosis-and-differential-diagnosis-of-parkinson-atm-s-disease.png)
The diagnosis of PD is clinical and requires bradykinesia, defined as slowness of movement and decrement in amplitude or speed, usually assessed using finger tapping, foot tapping or pronationsupination hand movements. In addition, rest tremor or rigidity is required to confirm a parkinsonian syndrome. Tremor was absent at presentation in 30% in one series of pathologically proven PD. Patients with suspected PD should be referred quickly and untreated to a specialist in movement disorders for evaluation. Key points for discussion at diagnosis include the need to inform vehicle licensing agencies and insurers, signposting to written or web-based information on newly diagnosed PD, and provision of contact details for the local PD nurse specialist .
Current International Parkinson and Movement Disorder Society diagnostic criteria for Parkinson’s disease adapted from Postuma RB, Berg D, Stern M et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 2015 30:1591601. At least two supportive criteria and no red flags required for a diagnosis of clinically established Parkinson’s disease. Conditions in italics should be considered if the corresponding exclusion criteria or red flags are present.
Read Also: How Are You Diagnosed With Parkinson’s Disease
Testing For Parkinsons Disease
There is no lab or imaging test that is recommended or definitive for Parkinsons disease. However, in 2011, the U.S. Food and Drug Administration approved an imaging scan called the DaTscan. This technique allows doctors to see detailed pictures of the brains dopamine system.
A DaTscan involves an injection of a small amount of a radioactive drug and a machine called a single-photon emission computed tomography scanner, similar to an MRI.
The drug binds to dopamine transmitters in the brain, showing where in the brain dopaminergic neurons are.
The results of a DaTscan cant show that you have Parkinsons, but they can help your doctor confirm a diagnosis or rule out a Parkinsons mimic.
Likelihood Of Referral According To Final Diagnosis
Overall, 74% of all cases with a diagnosis of Parkinson’s disease had been seen by a specialist. However, when these cases were classified by final diagnosis , it was observed that, paradoxically, fewer cases with atypical disease had been seen by a specialist compared with those with classical Parkinson’s disease p = 0.02).
Don’t Miss: Can You Drive If You Have Parkinson’s Disease
Neurodegeneration With Brain Iron Accumulation
Neurodegeneration with brain iron accumulation patients present with a progressive extrapyramidal syndrome associated with iron deposition in the basal ganglia. The two main syndromes are outlined here, although there are additional syndromes including neuroferritinopathy and aceruloplasminemia. The most common of the NBIA disorders is pantothenate kinase-associated neurodegeneration , resulting from mutations on the PANK2 gene, accounting for 50%. The classic syndrome manifests in early childhood with a combination of pyramidal and extrapyramidal features . PKAN can also rarely present in early adulthood. There are typical MRI findings, with a central hyperintensity with surrounding low signal on T2 images in the globus pallidus, giving the so-called eye-of-the-tiger sign .
The second main type of NBIA is PLA2G6-associated neurodegeneration . When onset occurs in infancy, PLAN causes progressive motor and mental retardation with cerebellar ataxia, seizures, and pyramidal signs. However, onset can occur later in life which leads to an atypical syndrome that may mimic PD, with rest tremor, rigidity, and bradykinesia and a good response to levodopa. However, patients also exhibit additional features including eye-movement abnormalities and pyramidal signs .
I Have Pd And Several Symptoms Should I Get A Datscan
Likely no. There is no need for DaTscan when your history and exam suggest Parkinsons disease and you meet the diagnostic criteria. Occasionally, if signs and symptoms are mild or you dont meet the diagnostic criteria, your doctor will refer you for a DaT scan. Keep in mind that ultimately the diagnosis is based on your history and physical exam. The DaT scan is most commonly used to complete the picture and is not a test for a diagnosis.
Don’t Miss: Do You Hallucinate With Parkinson’s
Advanced Therapies For Parkinson’s Disease
When significant off-time or dyskinesia persists despite optimised oral treatment, advanced therapies should be considered. Apomorphine, a potent dopamine agonist given by continuous subcutaneous infusion, is the least invasive and most straightforward of these. Following on from extensive clinical experience, the recent double-blind TOLEDO study confirmed a significant reduction in off-time and improved on-time with apomorphine versus placebo.
Deep-brain stimulation involves surgical placement of electrodes into brain regions such as the subthalamic nucleus to improve motor fluctuations or refractory tremor. DBS is typically considered in patients without significant axial or neuropsychiatric problems. It improves motor function, off-time and QoL in patients with PD, and provides significant benefits over medical therapy even in patients with an average disease duration of 7 years. The benefits of DBS on motor function, fluctuations and activities of daily living have been demonstrated up to 10 years postoperatively, although axial features continue to progress. Infusion of levodopacarbidopa intestinal gel via jejunostomy has also been shown to improve off-time compared to oral levodopa, and is commissioned in specialist centres where other advanced therapies are ineffective or contraindicated. Further information on the decision-making process for advanced therapies is summarised in a dedicated review.
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms noticed by the patient or his or her loved ones are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctors office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinsons disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Recommended Reading: What Is The Last Stage Of Parkinson Disease
Frontotemporal Dementia With Parkinsonism
Parkinsonism in frontotemporal dementia is usually seen in the behavioral variant, rather than in association with primary progressive aphasia, and can develop either before or during the development of the classical FTD syndrome. It can closely mimic idiopathic PD or have features suggestive of PSP or CBS. It is seen in association with underlying tau, TDP-43, or FUS pathology, as well as corresponding mutations in several genes, which include MAPT, PGRN, C9ORF72, FUS, and TARDBP. Rigidity and bradykinesia tend to be the more prominent parkinsonian features, with rest tremor occurring rarely. There is variable responsiveness to levodopa .
source https://www.parkinsonsinfoclub.com/diagnostic-criteria-for-parkinsons-disease/
